Atrial Fibrillation
Atrial fibrillation is a common heart rhythm condition where the upper chambers of the heart (the atria) beat irregularly and often rapidly. AF can be intermittent (comes and goes) or persistent, and it often progresses over time.
For most people, treatment is about three goals:
Feel Better
Reduce symptoms such as palpitations, breathlessness, fatigue, reduced exercise tolerance, dizziness, and poor sleep. Many people also feel better when their rhythm is stabilised and medication side effects are minimised.
Stay Safer
AF can increase the risk of stroke. Stroke prevention is often a core part of AF care and may involve blood thinners (anticoagulants). For selected patients who cannot take long-term anticoagulation (or have very high bleeding risk), left atrial appendage occlusion/closure (LAAO/LAAC) can be an alternative strategy.
Be Better Long-Term
For many patients, a rhythm-control strategy (aiming for normal rhythm) is increasingly important — especially if symptoms persist, AF is progressing, or AF is affecting heart function. Evidence supports early rhythm control in appropriately selected patients.
Treatment Options
1. Foundations: risk factors and triggers
Good AF control is more likely when contributors are addressed alongside any medications or procedures:
blood pressure control
sleep apnoea assessment/treatment
weight and cardio-metabolic health
alcohol reduction
fitness and conditioning
(These don’t replace medical therapy — they improve your odds of long-term success.)
2. Medications
Medication strategies usually fall into two categories:
Stroke prevention: medications used to prevent clots forming inside the heart during AF which lead to devastating strokes.
Rate/Rhythm control: anti-arrhythmic medicines aimed at reducing AF episodes or maintaining normal rhythm.
3. Electrical cardioversion
A short, controlled procedure to restore normal rhythm. Cardioversion can be used to:
relieve symptoms quickly
help determine how much better you feel in normal rhythm
support an overall rhythm-control plan
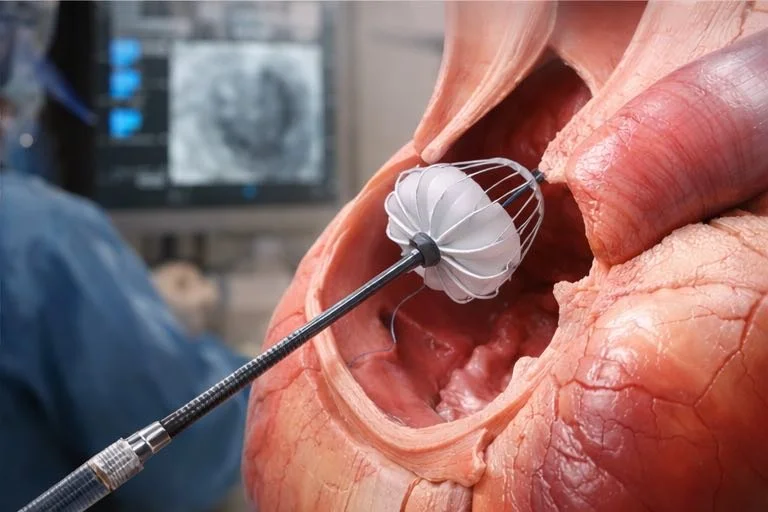
4. Catheter ablation
Catheter ablation — commonly pulmonary vein isolation (PVI) — is a minimally invasive procedure targeting the electrical triggers that initiate and sustain AF. It is a well-established rhythm-control therapy, including as first-line rhythm control for selected patients.
Energy types you may hear about
Radiofrequency (RF) ablation (thermal energy)
Pulse field ablation (PFA) (non-thermal “electroporation”)
PFA (Pulse Field Ablation)
PFA uses high-voltage electrical pulses to create non-thermal irreversible electroporation in heart tissue. Its major appeal is tissue selectivity — aiming to minimise injury to nearby structures (such as the oesophagus and phrenic nerve) compared with thermal approaches.
5. Stroke prevention alternatives
If you are at moderate to high stroke risk and long-term anticoagulation is not suitable due to bleeding risk or intolerance, percutaneous left atrial appendage closure (LAAC) may be considered. The procedure reduces stroke risk by sealing the left atrial appendage and can provide protection comparable to anticoagulation in carefully selected patients, without the need for lifelong blood-thinning medication.
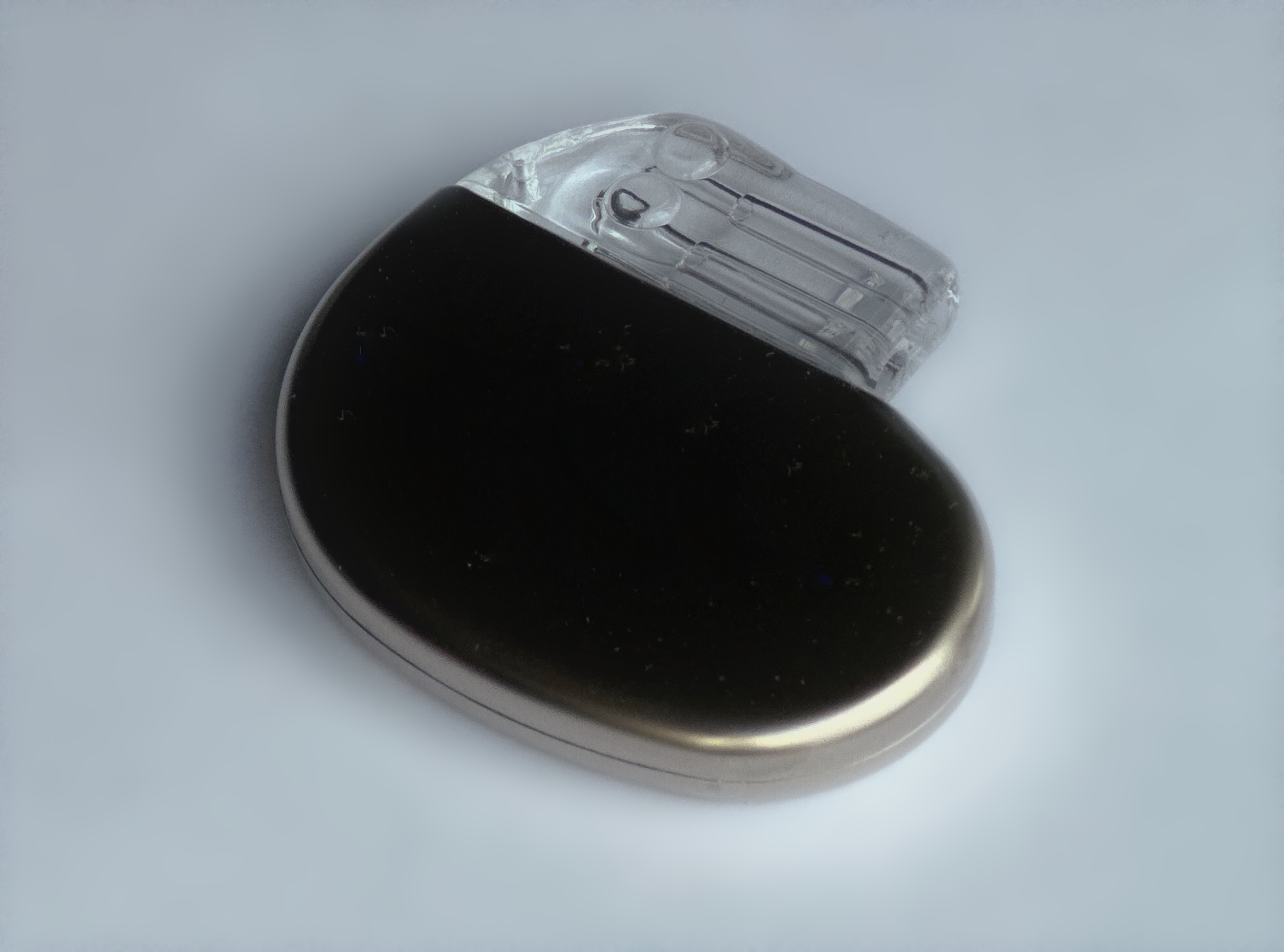
6. Pacemaker-based strategies
A pacemaker is not a routine AF treatment, but it can be part of an AF plan when:
necessary medications cause significant bradycardia, or
AF remains difficult to control and an AV node ablation + pacing (“pace-and-ablate”) strategy is appropriate for symptom control and rate control.
A simple way to decide what’s right for you
There is no single “best” treatment for atrial fibrillation — only the approach that best fits your heart, your risks, and your priorities at a given time.
Decisions are made through shared discussion, weighing symptom burden, stroke prevention needs, bleeding risk, AF pattern and progression, heart structure and function, and the potential benefits and risks of medications or procedures. For some, early rhythm control is appropriate. For others, careful monitoring and optimisation may be the better first step.
AF is often a dynamic condition. As circumstances change, your treatment strategy can be adjusted thoughtfully and safely.