Valvular heart disease
What it is
Your heart has four valves (aortic, mitral, tricuspid and pulmonary) that keep blood moving in the right direction. Valve disease means one or more valves don’t open or close properly, which can disrupt blood flow and make the heart work harder.
Most valve problems fall into two broad types:
Stenosis: the valve becomes narrowed and doesn’t open fully
Regurgitation: the valve becomes leaky and doesn’t seal properly
Symptoms
Some people have no symptoms for years, even with significant valve disease. When symptoms occur, they commonly include:
shortness of breath (especially with exertion)
chest tightness or discomfort
fatigue or reduced exercise tolerance
light-headedness or fainting
palpitations or ankle swelling
If symptoms are new, worsening, or occurring at rest, seek urgent medical review.
Causes
Valve disease can be caused by:
age-related degeneration and calcification (common with aortic stenosis)
previous rheumatic fever (still relevant for some valve patterns)
infection (endocarditis)
congenital valve variants (e.g., bicuspid aortic valve)
connective tissue disorders
How is it diagnosed?
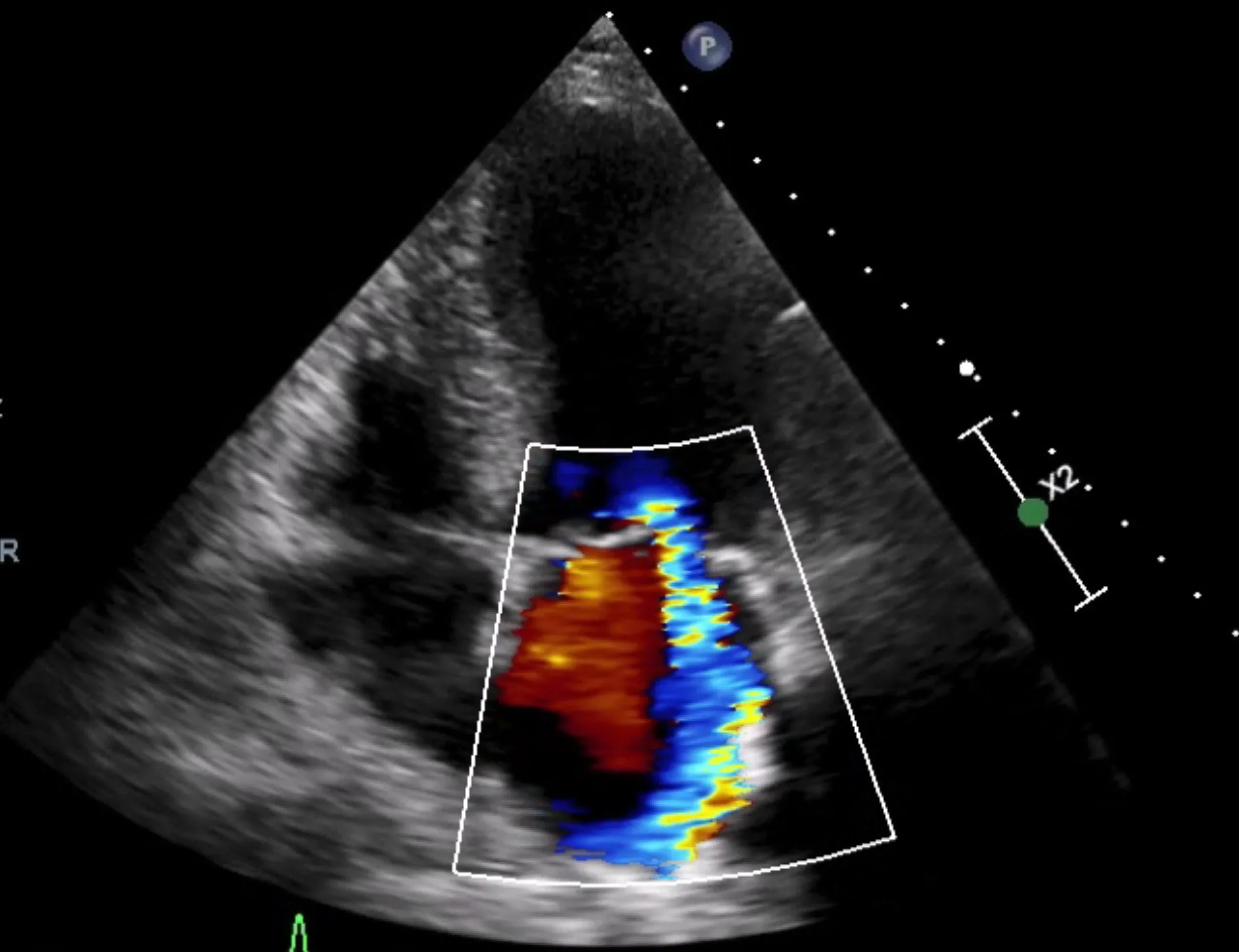
The key test is an echocardiogram (ultrasound of the heart), which assesses valve structure and severity and how the heart is coping.
Depending on the question, we may also use:
transoesophageal echocardiogram (TOE) for higher-resolution valve assessment
CT (useful for valve anatomy and planning transcatheter procedures)
cardiac MRI (helpful for volumes, function, and regurgitation assessment in selected cases)
Treatment Options
1. Monitoring (often the main treatment early on)
Many valve conditions are mild or moderate and are best managed with regular surveillance (repeat echo at intervals) and symptom review.
2. Medications (supportive, not a “cure” for the valve)
Medications can help control symptoms and treat the effects of valve disease (blood pressure control, fluid management, rhythm control), but most medications do not “fix” a severely narrowed or severely leaking valve.
3. Valve intervention (when severity and timing warrant it)
When valve disease becomes severe and/or symptoms develop — or when it starts affecting heart function — intervention may be recommended.
Options include:
Valve repair (often preferred when durable repair is feasible, especially for some mitral valve conditions)
Valve replacement (surgical or transcatheter)
Transcatheter therapies in selected patients (e.g., TAVI for aortic stenosis; catheter-based mitral interventions for selected cases)
4. A team-based decision
For severe valve disease where intervention is being considered, guidelines emphasise evaluation by a multidisciplinary heart team, balancing valve anatomy, symptom burden, heart function, age/frailty, procedural risk, and patient goals.